The importance of resilient workforce in social care and health sector owes to the fact that the health care workers face demanding situations on daily basis at workplace. Stressing out every day requires attribute of resilience as key component for working in healthcare settings. Angie Hart and Derek Blincow developed a framework of resilience (Appendix 1) that assists in strategizing and planning for creation of resilient members of the workforce. Resilience Framework combines a varied set of practices and ideas that assist in promotion of resilience, which is a fundamental part of resilient Therapy (RT), and supports research and practice of the profession. The complexity and vulnerability of health and social care professionals varies from the degree of stress, and profession, which requires structured response and intervention. For example, theory of ‘Resilience Engineering’ highlights strategies and plans that can assist incorporation of safety management plans within health and social care units. The incorporation of safety management plans assists in dealing with complex conditions, vulnerable threats, and disastrous situations. Emotional turmoil and work-related stress adversely impacts the efficiency of social and health care workforce. In the absence of resilience at healthcare workplace, professionals tend to shrink, rather than grow from stressful situations.
The pre-condition for a resilient health care workplace is establishing the culture that considers prioritizing of professionals working in stressful situation because well-being of all the stakeholders to health and social care services matter. Other professionals, such as medical practitioners and doctors, defines their moral values around working for making patients healthier, and not approach work as problem fixing mechanized work. The resilient point of views contribute to resilient workforce, which directly impacts the efficiency of health and social organizations in enhancing positive focus of the professionals working in the field. The assessment of potential threat and vulnerabilities in numerous possible situations can assist the process of devising capacity building training programs, along with new emergency planning processes, which inculcates resilience within organizational culture of social and health care sector. “All-Hazard Approach” is extremely useful in analyzing vulnerable situations, coupled with potential threats, within workplace settings of medical sector. Additionally, healthcare management relies on effectiveness through taking regular follow-ups of the plans that incorporate risks in accordance with management core principles. A well-coordinated and efficient care system, which relies on meeting the patient needs, through mitigating the future vulnerabilities facing health care providers within framework of emergency systems.
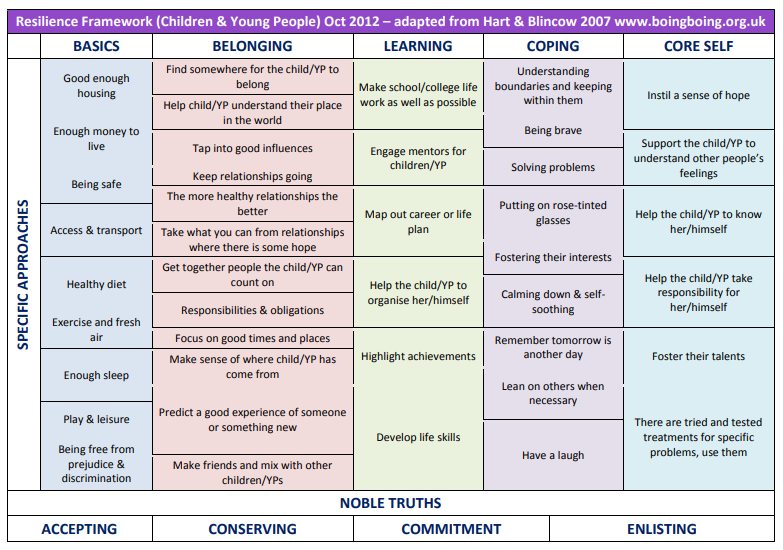
Furthermore, assisting in maintenance and development of communication plans that shows resilience in healthcare providers work culture. The adaptation of resilience approach on part of health and social care providers requires inheriting the value of resilience as permanent adaptation of work-life and personal life. The benefits of resilience in workforce means a resilient culture at workplace. Organizational culture is multilayered, and the foundations of it relies on purpose, empowerment, accountability, and trust. One of the experience that I faced during my work at healthcare settings is the complexity of schedules that lowers the efficiency in longer run, especially the level of resilience. Resilience flourishes in feasible environments where belonging, learning, basics, core self-beliefs, and coping strategies stay intact. One of the primary factor contributing to low resilience at workplace is the reduced amount to sleep, which negatively impacts the productivity of health workers, especially in times of health emergencies. Additionally, one of the key factor at the organizational culture is prejudices and discriminations. Although, healthcare center attempts to create prejudice and discrimination free workplace for workers, the constant interaction with patients results in socialization that sometimes result in unhealthy interactions. Racism is one of the rising issue in the country with higher prevailing rates for basic needs, which includes health care sector that is extremely expensive in the developed world.
Reflection No. 02: Resilience and Workforce of Health and Social Care
The promotion of resilience at workplace depends on cultivation of attention and awareness, which means higher level of personal awareness in terms of emotional intelligence, and ensuring rational response to the outside world. The awareness is in absolute terms, and follows an inclusive approach towards varied aspects of life, which includes ‘self-care’ as central component to the recovery process. For example, three-step breathing practice in vulnerable situations allow for the creation of vacuum between responses and feelings, which results in effective management of emotions and rational argumentation. The continuation of healthcare services in times of COVID-19 pandemic requires catering to the emotional wellbeing needs of public health practitioners. On the contrary, healthcare providers are under psychological pressure at work which are going to impact mental health of health care providers. The psychological resilience of healthcare professionals during pandemic times require enhanced level of personal care, that is, in terms of life satisfaction, positive emotions and quality of sleep. Experienced professionals tend to show more resilience during stressful times of pandemic, while sleep remains the primary determinant of life satisfaction, quality of life and resilience at the psychological level of health and social care workers, which constitute doctors level as lowest amongst variety of categories within healthcare workers.
During COVID-19, attending work while ill, presenteeism is a strong phenomenon which negatively impacts productivity of the employee, and subsequently productivity of the employer in providing health and social care services. Overall, the cost of presenteeism phenomenon is greater when compared with absenteeism. Presenteeism is a recurring phenomenon for at least once a year, and the rising depression and anxiety levels during pandemic suggest that the presenteeism is not affordable to the health care centers. Promotion of resilience results in reduced frequency of presenteeism. Generally, high stress levels are associated with rising figures for presenteeism, and absenteeism. Unlike presenteeism, absenteeism is the result of disengagement at work, or physical and mental illness that results in employee taking leave from work, and physically absent at work. Absenteeism during COVID-19 increases due to lack of proper care needed by healthcare workers to maintain their mental and physical wellbeing. However, presenteeism during pandemic have increased due to heavy workloads, and job security is not the major because the demand for healthcare professionals is high during health emergency state worldwide. Trainings for increasing resilience of the workforce in healthcare settings positively impacts, and decreases the ratio of presenteeism and absenteeism. The direct and positive relationship between resilience and presenteeism/absenteeism suggest that the design of ‘resilience training programs’ within healthcare units as part of the strategy to uplift wellbeing of health workers is the way forward for increasing organizational productivity of the healthcare organizations.
Organizations that supports to address resilience, and shows commitment in their company-wide statement results in strengthening of the resilient culture at workplace. One of the critical role played-in by the mid-level employees that works as a chain between the top-tier leadership and operations or low-tier employees, which is, playing an effective role as facilitator of trust and openness, and considering the mental well-being of the staff as central component of the organizational culture. Healthcare and social care organizations work tirelessly, especially during COVID-19 to embrace values of resilience for workers because they are at the frontline of fight against the pandemic. The quality of work improves, and health workers are more encouraged to use the autonomy of work and organizational trust at their advantage in providing relief to the patients. However, providing access to support and services are crucial to the wellbeing of health workers, especially doctors that are on the front line of fight against pandemic, which also reflects the low resilience for medical practitioners during COVID-19.
Reflection No. 03: Encouraging Resilience at Workplace
Workplace stressors plays a negative role in work efficiency of the healthcare worker because long hours, changes to schedules, and other similar factors can be significantly contributing to the overall work productivity of the organization. However, autonomy at work is positively associated with creating resilience, and this is possible when the health care workers are equipped with the skills needed for maintaining resilience at work. For example, autonomy of time assists in discarding distraction created within hierarchical structure of the organization, but it requires high capacity of the health providers in empowering workers to ensure patient-friendly health services at first place. The role in encouraging resilience at workplace relies on the support for each other, and building an atmosphere that becomes ecosystem for growth of resilience at workplace. Showing support for the work of health workers, and acknowledging the efforts in the form of effective reward system serves the purpose of motivating employees. Motivation is also another factor that is central to the concept of resilience because it assists in the formation of mindful worker with confidence in the organizational culture and profession. Motivation enhances individual focus at workplace, and assists in possessing leadership skills that other might want to follow. A resilient person encourages others around with the attitude of a discipline, mindful, compassionate, and well literate in communication. For example, outbreak of COVID-19 pandemic has changed the workplace in drastic manner as it reflects the higher demand for services, and consequently long hours of work shifts that severely hampers the resilience of health workers. Doctors, on the other hand, requires additional support due to low resilience levels during current pandemic, which is primarily link to work burden and horrifying state of health-emergency. The required support for doctors, and other healthcare practitioners directly working with patients, aims to strengthen resilience because it positively contributes towards overall health care service delivery.
Team development, and understanding dynamics within team is extremely useful for accelerating the process of resilience building. There exists various methods for creating resilience among healthcare workers, which includes supervision, and mentorship. Mentorship and supervision are slightly different, however they both overlaps. Mentorship and supervision allows for development of proficiency in mindfulness, distress tolerance, and positive framing as critical skills for reflective discussions based on Resilience Based Clinical Supervision. In a healthcare organization, care for each other concerns, coupled with assisting each other at employee levels, and establishes the core values that strengthens resilience. The role of mentor in healthcare settings takes place between the hierarchical mobility of workers, which means each person mentee and mentor at the same time for two or more people. Resilience is strengthened with lending hand to each other with the introduction of required skills and expertise for the job. Mindfulness, distress tolerance, and positive framing are central to the process of mentoring because if the resilience is the core value then eventual outcome is higher work productivity. Mindfulness is the ability to be oneself now with the required focus to perform the task, and especially without mental and physical exhaustion. For example, lack of sleep in quantity and quality, coupled with long hours of work results in distracted thoughts that results in lack of efficiency. The overall pattern of growth of resilience in workforce is the result of compassion and care for each other, especially during pandemic times. Supervision allows for another assistance methodology that a health worker can provide to another health worker when support is required. Lending hand at work during health emergency to each other in healthcare settings increases the overall satisfaction of patient, while creating an atmosphere of supporting resilience. The support of each other at healthcare settings establishes norms and values in group dynamics of organizational culture that promotes resilience at work, which is also associated with overall satisfaction of the patients.
Reflection No. 04: Leadership Skills and Resilient Workforce of Health and Social Care
The way forward for the healthcare staff during work is to become vessels for facilitation of patients in improving health conditions, which is also central to the job of healthcare workers. Management of health and social care organization needs to prioritize the facilitation of the workers through programs that focus on stress management, coupled with health management. A central component of health management programs, in terms of injecting resilience in the workforce, are aimed at strategizing training programs that focusses on tasks and activities like meditational sessions, stress check, and motivating employees to regularly maintain short walks. Emotional bank balance is the net-emotional worth of an individual after netting-off for withdrawals. For example, a health worker can criticize for certain thing, and can interrupt others when they speak during emergency. A healthy work environment ensures the emotional bank balances of health workers as positive balance, that is, emotional deposits are higher than the withdrawals. Leadership skills are also central to making deposits in emotional bank account of the subordinates because it flourishes culture of depositing, instead of withdrawing. However, humans do make mistakes, and if the emotional balances are always high within the organizations, then the immediate impact is in the form higher level of tolerance and patience.
Leadership task is to assist employees in sustaining sufficient balance in the emotional bank account for flourishing the culture of trust, compassion, duty, empathy, and care for each other during health care service delivery, which requires preparation on part of healthcare providers. Most common withdrawals are in the form of criticizing someone, back-biting, long screen-times, sarcastic comments, etc. On the other hand, emotional deposits in the bank account of healthcare workers can be in the form of apologizing for a mistake without giving concern for humility. Additionally, greeting them upon there successful achievements, while assisting them when asked for professional or personal assistance. Additionally, patients and gentle attitude at healthcare work atmosphere assists in establishing strong culture based on resilience. An effective leader can inculcate resistance through setting direction for healthcare workers in terms of meaningful goal, especially something that is higher than personal gains like salary package or repute. Self-awareness of leader assists in advocating for higher level of self-awareness, and mindfulness, which is an extremely useful strategy for establishing solid footings for resilience at workplace. Leaders set norms and values for the organizational culture, and strengthening resilience through strong leadership requires social support of leader themselves at personal level vis-a-vis the health care workers.
My experience with leadership in healthcare placed me at odds with the required fast-faced work style, which requires at the same time multiple facets to perform the tasks. For example, setting meaningful goal for personal self, which is higher than the ego. The primary purpose of healthcare workers is to facilitate the process of leading the team where each worker understands the role they play within the healthcare service delivery system. Self-awareness, and acting wisely regardless of the stressful situation requires attachment and detachment of the health worker at work simultaneously. It is important to be aware of the self, and the distinguishing of work and personal with compassion and empathy for each other. A leader acts wisely in rough situation because there is no room for him or her to fail due to his presumed leadership position. A strong leader sets the example by stepping up to the toughest job at hand for creating resilience, confidence, morale, and faith of individual health worker. Personally, leadership position provides more opportunity to understand individuals in top of the hierarchy, and karma is at play when assisting each other at above and below the organizational hierarchy. Leadership reflects in the service delivery process, and people are more motivated to work with higher productivity without presenteeism and absenteeism.
Bibliography
Bozdağ, F., & Ergün, N. (2020). Psychological resilience of healthcare professionals during COVID-19 pandemic. Psychological reports, 0033294120965477.
Howe, D. (2008). The emotionally intelligent social worker. Macmillan International Higher Education.
McCray, J., Palmer, A., and Chmiel, N. (2016). Building resilience in health and social care teams.
McFadden, P., Mallett, J., and Leiter, M. (2018). Extending the two‐process model of burnout in child protection workers: The role of resilience in mediating burnout via organizational factors of control, values, fairness, reward, workload, and community relationships.
Robertson, H. D., Elliott, A. M., Burton, C., Iversen, L., Murchie, P., Porteous, T., & Matheson, C. (2016). Resilience of primary healthcare professionals: a systematic review. British Journal of General Practice, 66(647), e423-e433.
Woods, D. (2006). Engineering organizational resilience to enhance safety: A progress report on the emerging field of resilience engineering. In Proceedings of the human factors and ergonomics society annual meeting.
Appendix 1: Resilience Framework
Figure 1
https://www.boingboing.org.uk/resilience/resilient-therapy-resilience-framework/