Adult bronchial asthma is characterized by chronic airway inflammation, clinically presenting variable airway narrowing, and associated with bronchial hyperresponsiveness and chronic airway inflammation. Asthma is a chronic inflammatory disorder of the airways, a common and potentially serious chronic disease that is associated with variable expiratory flow, airway wall thickening, respiratory symptoms, and exacerbations (Kostakou et al., 2019). Asthma is commonly seen in childhood and affects anyone despite age or gender. Asthma takes place in two forms; acute and chronic. Acute asthma exacerbation known as an asthma attack is a progressive worsening of asthma symptoms which includes shortness of breath, wheezing, cough, and chest tightness. In acute exacerbation of asthma PEF is 33–50% best or predicted, respiratory rate ≥ 25/min, heart rate ≥ 110/min, and inability to complete sentences in one breath (Kostakouet et al., 2019). Chronic asthma develops due to the changes that occur from prolonged inflammation and develop gradually (Huether & McCance, 2017). Asthma is a consequence of complex gene and environment interactions. According to the Global Asthma Report, approximately 334 million people in the world suffer from asthma. The latest World Health Organization (WHO) estimates, released in December 2016, present that there were 383,000 deaths due to asthma in 2015(Kostakou et al., 2019).
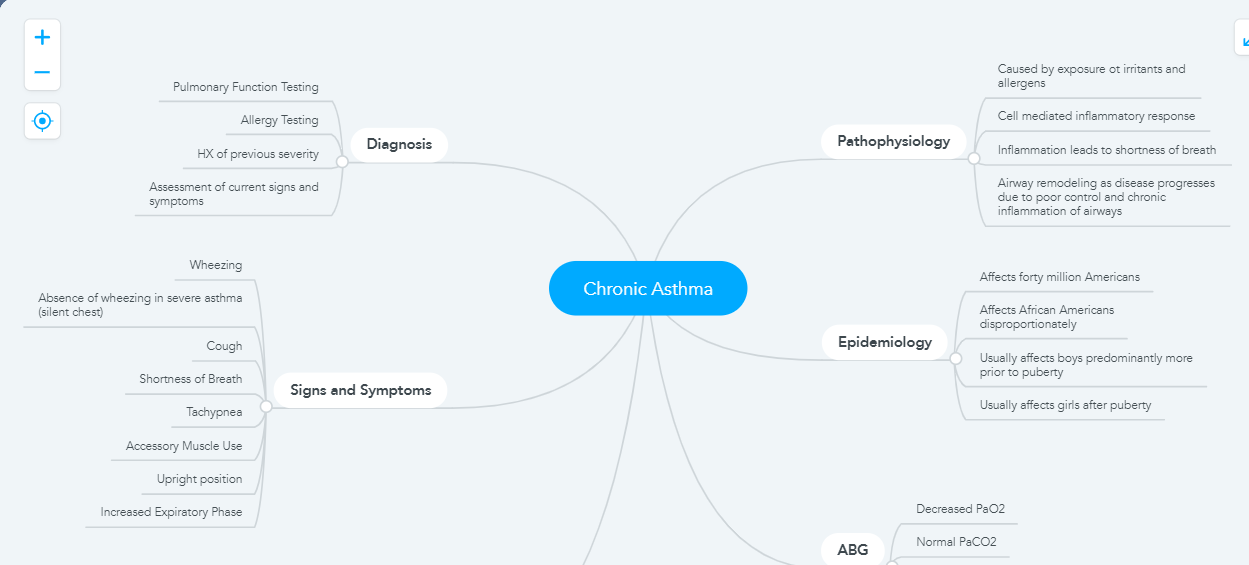
Pathophysiology of chronic asthma
Chronic asthma is caused by the prolonged existence of some recurrent symptoms of the disease for a long time, which is closely associated with etiological aspects of Chlamydia and persistent viruses. The repeated occurrence of inflammation in bronchi and bronchioles results in to increase in the smooth muscle layer of the airway and raise the sensitivity to allergens. The increased inflammation and release of cytokine may mark the presence of chronic asthma. These cells contain immune cells such as macrophages and eosinophils. The increased sensitivity of the airway is caused by the growth in the eosinophil level in the lamina propria. Further blockage of the airway during the asthmatic attack is due to the variation related to chronic asthma that leads to the rise in several mucous glands in the airway(Gelb et al., 2016). Drugs used for asthma can easily reverse asthmatic attacks because these drugs reduce inflammation and cause changes in the airway. In the case of chronic asthma, oxygenation is not proper due to restriction of the bronchial airway. Reduction in the level of oxygen in the arterial blood resulted from the lower oxygenation of blood in the lungs. The blood gas of arteries is affected by hyperventilation caused by hypoxemia which leads to respiratory alkalosis. According to Huether & McCance, (2017) the Pa02 is decreased and the Ph value rises up to 7.4 to 7.45 which leads to respiratory alkalosis.
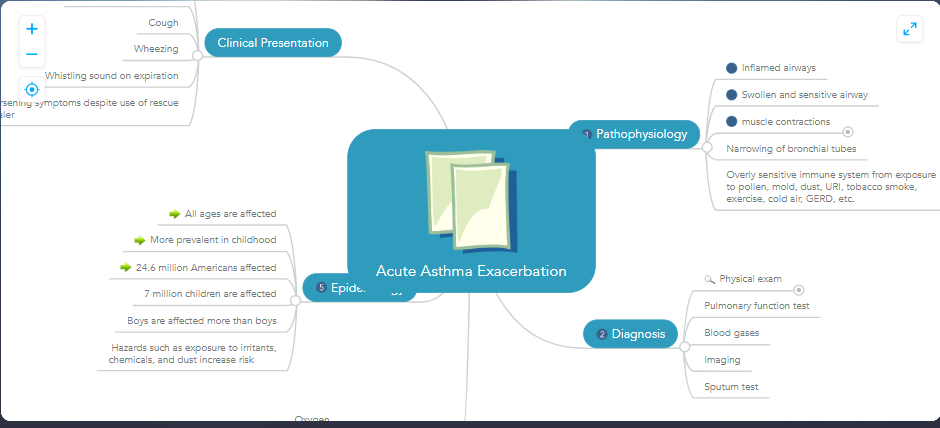
Pathophysiology of acute asthma exacerbation
The “2014 British Guidelines for Asthma” defined acute severe asthma as asthma exacerbation which is presented with one of the subsequent conditions: PEF 33 to 50 % predicted or best. The respiratory rate is greater than 25/min, the heart-rate is greater than 110/min, and the patient with the incapability to ample a sentence in a single breath. Acute-asthma-exacerbation is identified by the rescindable bronchoconstriction and airway resistance is increased. The rate of flow is low, and the airway closure is small and premature. Moreover, pulmonary hyperinflation and elastic recoil decrease, and the work of breathing increases (Gelb et al., 2016). In acute severe asthma, the arrangement of ventilation-perfusion is bi-modal, it ranges from normally perfused parts to the areas of hypoxic-pulmonary-vasoconstriction. The ventilation or perfusion mismatch (V/Q mismatch) in acute exacerbation of asthma results increase in blood flow, the cardiac output is high, and dispersed in alveolar spaces along with lower airing and an unusually lower ratio of V/Q.
Asthma exacerbations consist of episodes of asthmatic attacks identified by the worsening of asthmatic signs that include shortness of breath, chest tightness, and wheezing. It is mostly caused by weather changes, exercise, allergens, drugs, emotional expressions, and dehydration (Papi et al., 2018). Inhalation of certain substances which cause inflammation in the airway such as smoke or dust causes inflammatory mediators from the airway’s walls leading to the worst asthmatic attack. Repeatedly occurrence of acute asthmatic attacks should be avoided as it can lead to the development of chronic conditions of asthma, and persistence of the condition. Acute attacks can aggravate chronic asthma. The patient requires immediate treatment of resultant symptoms that may be helpful to avoid chances of development of complications and sustaining further damage to airways. Arterial blood gas (ABG) measurement can provide helpful information in acute asthma. The prevailing ABG findings during acute asthma exacerbation are the causes of hypoxemia which results in hyperventilation and respiratory alkalosis. Prolonged asthma attacks result in further accumulation of CO2 gas that increases partial pressure in the arterial blood (Durham et al., 2017). Evaluation of this partial pressure of both inhalation and exhalation of oxygen and carbon dioxide gases prior to and post-treatment could be a good source of progress. Heuther and McCance (2017) argued that oxygen therapy is advised to be conducted carefully to avoid respiratory alkalosis which is initially caused by hyperventilation of the alveolar.
Impact of Genetics as a Factor on Acute Asthma Exacerbations
A genetic factor is very important in asthma, as the children of asthmatic parents are highly vulnerable to asthma. Different studies examined polymorphism for IL2RB9, IL33, SMAD3, HLA-DQ, and IL1RL1/IL18R1, furthermore, the locus on chromosome 17q21 containing the genes ORMDL3, GSDMB, and ZPBP2 are connected in epithelial hurdle function and inborn and an adaptive-immune replies in asthma. In my class, I major histocompatibility complex controlled T cell related with CRTAM molecule gene was linked with the high rate of asthma exacerbations in the kids with a lower level of flowing vitamin D and TT allele at rs7216389 has an association with proportion of 1.6 (the odds ratio) of having the asthma-exacerbation when it is associated with the CC allele. Kostakouet et al., (2019) stated that the polymorphisms for FCER2 are related to a lesser number of FCER2 gene manifestations, higher levels of serum IgE soar the possibility of strong exacerbations.
Diagnosis of Acute Exacerbation of Asthma
For the treatment of asthma, the victim is required to provide a complete family and personal medical history, chest and sinus x-ray, physical examination, and lung function test (LFT) for measuring breathing. LFT is often done twice, once before treatment and then after inhaling medicine such as a bronchodilator that opens the airways. It is examined that if the lung function is improved significantly by using this medicine, that confirms the diagnosis of asthma. Kostakou et al., (2019) argued that the Lungs Function Test includes the Feno test, allergy test, spirometry test, provocation test, blood test, peak airflow, and spirometry test.
Treatment of Acute Exacerbation of asthma
There are two ways the treatment of asthma patients; one is through medication, while others are non-pharmacological treatment plans. In non-pharmacological treatment patients are educated and aware of self-monitoring of symptoms of the disease, a written plan is provided to take the right action for controlling the level of pain, which will let them timely acknowledgment and organization of exacerbations and know about their regular medical reviews. The mild to moderate level of asthma requires pharmacological treatment which includes short-acting beta-agonists or SABA, oxygen therapy, and prednisone. For severe asthma exacerbation patients are advised to treatment including Leukotriene receptor antagonists (LTRAs), Corticosteroids, SABA, methylxanthines, Anticholinergics, anti-IgE, chromones, anticholinergics, and oxygen supply (Kostakou et al., 2019)
Treatment of Chronic asthma
The following steps are required for the treatment of chronic asthma.
Step 1 (intermittent)-SABA as required (PRN), also the recommended treatment is needed for patients at this level since they show only intermittent signs.
Step 2(mild persistent)- For mild and persistent asthma, at this level, the patient is advised to take a low dose of SABA, and ICS is needed.
Step 3 (moderate persistent)- Low to medium dose of ICS and a low dose of LABA.
Step 4 (moderate persistent) – An increased dose of ICS should be given to the patient, also LABA may be given at this point.
Step 5 (severe persistent) – High dose of ICS, LABA, and Omalizumab is required for the patient at this stage as the patients with allergic asthma are having allergic asthma.
Step 6 (severe persistent)- At this stage patients require a high dose of LABA, oral CS, and ICS. For patients having allergies omalizumab should be considered, and oral corticosteroids are needed. (Arcangelo et al., 2017).
Mind Map of Acute and Chronic Asthma
References
Arcangelo, V., Peterson, A., Wilbur, V., & Reinhold, J. (2017). Pharmacotherapeutics for advanced practice: A practical approach (4th ed.). Philadelphia, PA: Wolters Kluwer.
Durham, C. O., Fowler, T., Smith, W., &Sterrett, J. (2017). Adult asthma: Diagnosis and treatment. Nurse Practitioner, 42(11), 16–24. https://doi- org.ezp.waldenulibrary.org/10.1097/01.NPR.0000525716.32405.eb
Gelb, A. F., Christenson, S. A., & Nadel, J. A. (2016). Understanding the pathophysiology of asthma–chronic obstructive pulmonary disease overlap syndrome. Current opinion in pulmonary medicine, 22(2), 100-105. doi: 10.1097/MCP.0000000000000236
Huether, S. E., & McCance, K. L. (2017). Understanding pathophysiology (6th ed.). St. Louis, MO: Mosby.
Kostakou, E., Kaniaris, E., Filiou, E.,Vasileiadis, I., Katsaounou, P.,Tzortzaki,E … Rovina. N. (2019). Acute Severe Asthma in Adolescent and Adult Patients: Current Perspectives on Assessment and Management. Journal of Clinical Medicine, (9), 1283. https://doi-org.ezp.waldenulibrary.org/10.3390/jcm8091283
Papi, A., Brightling, C., Pedersen, S. E., &Reddel, H. K. (2018). Asthma. The Lancet, 391(10122), 783–800. https://doi.org/10.1016/S0140-6736(17)33311-1